at a glance
Peony and PCOS: Could this be the missing link to help you ovulate?
Table of Contents
- 01 - Thyroid, Hormones, and PCOS - A Basic Overview
- 02 - When something goes wrong with the communication signals
- 03 - What are symptoms of Hypothyroidism?
- 04 - Prevalence of Thyroid Dysfunction in PCOS
- 05 - Symptom Overlap and Metabolic Function In Hypothyroidism and Polycystic Ovary Syndrome
- 06 - Insulin Resistance, Thyroid and PCOS - The Interplay
- 07 - Hypothyroidism and Pregnancy
- 08 - What are normal lab values for thyroid lab work in pregnancy?
- 09 - Can I take T3 thyroid medications in pregnancy?
- 10 - Thyroid Treatment in Pregnancy - Summary
- 11- What role does the thyroid play in preconception and fertility?
- 12- Fertility, PCOS and Thyroid Conditions
- 13- Brief Menstrual Cycle Lesson & Typical PCOS Cycles
- 14- Fertility Requires More than Ovulation
- 15- How Can I Advocate for Thorough Lab Testing and Thyroid Treatment with My Doctor?
- 16- Who should advocate for more thorough thyroid lab testing?
- 17- How Can I Convince My Doctor to Run These Labs?
- 18- What if the tests come back "normal" or close to it?
- 19- A Case Study of Subclinical Hypothyroidism and Fertility
- 20 - DISCLAIMER
I wrote before on Thyroid Health and Polycystic Ovary Syndrome. If you are interested in starting with an overview, check out that article here. In this article we are going to look at the thyroid in light of fertility and pregnancy more specifically with PCOS.
There is a good amount of debate over optimal thyroid levels in PCOS while trying to conceive. It can be a difficult subject to wrap your arms around and even more difficult to articulate your concerns when advocating for comprehensive care with your physician.
First of all, PCOS is what we call a diagnosis of exclusion meaning: in order to obtain a PCOS diagnosis you have to meet certain criteria but, you also need to have other disease states ruled out.
This is because there can be other explanations for a lack of menstrual cycle, anovulation and high levels of androgens. One of the conditions that should be ruled out is hypothyroidism. (1)
Before we dive into the science, let’s just review some basics and some statistics around thyroid health and PCOS.
Thyroid, Hormones, and PCOS – A Basic Overview
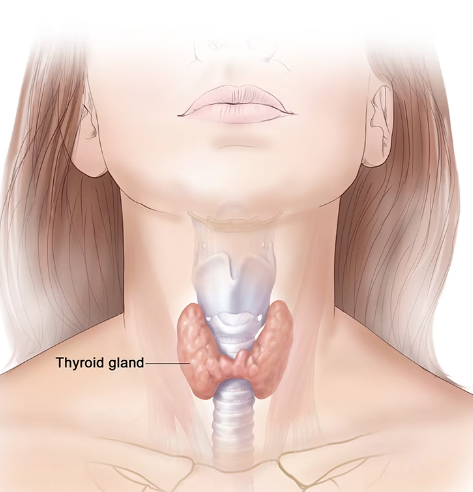
Your thyroid is an organ that sits towards the front of your neck. It is typically described as a butterfly shaped organ.
The primary function or purpose of the thyroid is to control the metabolic thermostat of the body. It receives a message from the pituitary gland of the brain via a hormone called ‘Thyroid-stimulating hormone’ or TSH. When your body sends more TSH to the thyroid, it turns on the production of thyroid hormone. When TSH levels go down, the thyroid creates less thyroid hormone.
Thyroid hormone is different than TSH. It is typically referred to as T4 (thyroxine) and T3 (triiodothyronine). Your thyroid makes T4 and then sends it out into the body and it is further converted into T3 in the liver. Basically an iodine molecule is removed from the hormone. Instead of having 4 of those, T3 only has 3.
T3 is the active form of thyroid hormone. Without going too far into the weeds you will sometimes see things written on labs like Free T4, Free T3 or even Reverse T3.
When a hormone is noted as ‘free’ like free T3 or free testosterone it means it is not connected to a carrier protein and is free to interact with different cells in the body and do its job sending a message. (2)
To summarize: Your brain makes TSH to tell your thyroid to make T4, then T4 is secreted in the blood and transformed into T3 in your liver. T3 is then sent around the body to do it’s job, impacting metabolism, digestion, hair growth, sex hormone production, ovulation and so much more!
When something goes wrong with the communication signals
Thyroid hormone receptors have been found on almost every type of tissue and cell in the body. When things go awry it can have widespread effects.
When your brain makes more TSH (ie you would have higher levels) it is working harder to get the thyroid to make enough thyroid hormones. The interesting thing is you can have an issue with this process in a lot of different areas.
Your thyroid can struggle to respond and make enough T4 or downstream your liver could have difficulty converting T4 into T3 (the active form of thyroid hormone). T3 is released from the liver and sent around the body to communicate with cells. These target tissues may struggle to respond to T3.
An issue with any of these could result in a diagnosis of hypothyroidism or an under-active thyroid.
There is another way things can go wrong and that is when the thyroid is over-reactive and making too much thyroid hormone. This is less common and much less common in the PCOS population, so this article will focus more in depth on hypothyroidism and PCOS.

What are symptoms of Hypothyroidism?
Hypothyroidism, when the thyroid is under-active, can express itself in symptoms like:
- making weight loss more difficult
- increasing hair loss
- impacting menstrual cycle regularity
- brain fog
- fatigue
- lower metabolic rate
- low mood and depression
- muscle weakness
- infertility

Prevalence of Thyroid Dysfunction in PCOS
You may have heard of something called subclinical hypothyroidism(SCH). This is when thyroid hormone levels appear normal but there is a mildly elevated TSH level. I have found it is important when considering something like subclinical hypothyroidism that we aren’t only looking through the lens of lab work, but at the patient in front of me and the constellation of symptoms they present with.
In one study comparing women with PCOS to a control group found that 43.5% of the PCOS group had subclinical hypothyroidism(SCH), while only 20.5% of the control group did. (3) In a study looking at 4065 women with PCOS aged 12-40 (reproductive age) a diagnosis of SCH was associated to obesity, central obesity, higher fasting glucose and higher HOMA-IR scores.
Hypothyroidism is where the disfunction is more severe and warrants a full thyroid diagnosis. Recent studies have reported that women diagnosed with PCOS have a higher incidence of hypothyroidism. In these studies the 11-14% of women with PCOS have hypothyroidism whereas age-matched controls only have rates of 1-2%. (4)
When we consider hypothyroidism, the greatest cause of hypothyroidism is an autoimmune thyroid disease called hashimoto’s thyroiditis (HT). In a systematic review including studies published until August 2017 13 studies were analyzed which included 12010 women with PCOS and 987 controls. The prevalence of HT was 26% in the PCOS group and only 9.7 % in the controls. That means there was a threefold increase in the prevalence of hashimoto’s thyroiditis in PCOS relative to the controls. (5)
In another study conducted of women of childbearing age 22.1% of PCOS patients had HT and only 5% of the control group. (6) It might make you wonder if the opposite is true. Are you more likely to have a PCOS diagnosis if you have hashimoto’s? The answer is yes, in one study 46.8% of patients with HT had PCOS, while controls that did not have HT only had 4.3% of the group diagnosed with PCOS.(7)
Symptom Overlap and Metabolic Function In Hypothyroidism and Polycystic Ovary Syndrome
If you were diagnosed with either hypothyroidism or PCOS you may experience hair loss, inability to lose weight, insulin resistance, dyslipidemia, increased weight, obesity and infertility. Individuals that have both diagnosis’ tend to have these symptoms to a larger degree.
Metabolic changes are observed in both polycystic ovary syndrome and low thyroid function whether overt hypothyroidism or subclinical hypothyroidism. These metabolic changes fall in the category of central adiposity(where the waistline is greater than hip circumference), higher BMI, weight, fasting blood sugar, HOMA-IR scores, cholesterol, and fasting insulin levels.
When hypothyroidism or SCH is treated with thyroid medication signs of metabolic disorder significantly improve. (8) PCOS patients with subclinical hypothyroidism have a higher HOMA-IR index(this is an index to compare levels of insulin resistance) compared with BMI-matched PCOS controls. This signifies that having an under-active thyroid can make insulin resistance worse.
PCOS patients with overt hypothyroidism had the highest levels of HOMA-IR. The good news is that the HOMA-IR levels decreased as thyroid treatment was initiated. (9) The key takeaway here is to get thorough lab testing and thyroid medication for treatment.
Insulin Resistance, Thyroid and PCOS – The Interplay
Insulin resistance is a core issue in PCOS. The communication that happens between cells and insulin is impaired and thus a woman with PCOS compensates by making more and more insulin.
Thyroid hormone has a role in blood glucose regulation. T3, which is a thyroid hormone regulates glucose synthesis in the liver. T3 also impacts the skeletal muscle tissue’s creation of glucose transporter proteins on the edge of the cell.
There is a strong correlation between higher levels of TSH and insulin resistance. (10)
Treatment of hypothyroidism is important in preconception, infertility, and pregnancy. We are going to discuss pregnancy first and then move backward from there so you can see how important optimal thyroid function is during this time.
Hypothyroidism and Pregnancy
In early pregnancy a baby depends on its mothers production of thyroid hormone. At about 12 weeks gestation the baby’s thyroid will start functioning but it will still rely on its mothers production of thyroid hormone until about 20 weeks of pregnancy. (11)
Much of babies early development in its brain and nervous system requires adequate thyroid hormone. (11) It goes without explanation that pregnancy itself is a state that requires high amounts of metabolic function. Consider the blood volume increases, increased caloric needs to grow a human and tissues to support all of this like a placenta.
Having hypothyroidism in pregnancy can have grave outcomes if it goes untreated. If untreated hypothyroidism can cause (11):
- miscarriage
- stillbirth
- low birthweight
- increase risk of preeclampsia
I know that list is pretty scary. The great news is we have gotten very good at treating hypothyroidism in pregnancy with medications that essentially provide your body more thyroid hormone. The most common medications are called levothyroxine and synthroid.
I have met and worked with many women and couples that would like to approach fertility and pregnancy from the most natural state possible. This is one of those areas I will always advocate for swift pharmaceutical interventions because the risks are just too high to gamble with.

What are normal lab values for thyroid lab work in pregnancy?
What are normal lab values for thyroid lab work in pregnancy?
Pregnancy is a metabolically expensive time in a woman’s life. Because of this our TSH levels will almost always increase after conception.
Most often doctors will only test TSH lab values and skip testing T4 or T3. If you have already received a hypothyroidism diagnosis you may be monitored more closely and thoroughly. Many physicians will order a lab called TSH with Reflex. This means if the TSH lab value is too low or too high the lab will then immediately run T4 levels to see if those levels are also out of range.
Since most doctors will screen TSH only that is what most of the lab values and treatment protocols in pregnancy are centered around. The needs change by trimester and by your baby’s ability to create and use its own thyroid hormone thus reference ranges are trimester specific.
First Trimester: .01-2.5 mIU/L
Second Trimester: 0.2-3.0 mIU/L
Third Trimester: 0.3-3.5 mIU/L
These values were taken from 2011 American Thyroid Association Guidelines. (12)
According to the American Endocrine Society treatment with T4 (levothyroxine) is recommended if lab values of TSH are higher than 2.5 mIU/L in first trimester or higher than 3.0 mIU/L in second or third trimester. (12)
One thing I have gathered from working with many infertility patients that go on to become pregnant is that this early screening of thyroid is not routinely happening and is often something the patient needs to firmly request with their provider.
High levels of TSH have been associated with an increased risk of spontaneous miscarriage and as such, it is my recommendation to have lab work done early in pregnancy between 5-8 weeks gestation and again every 4-6 weeks to ensure the thyroid levels are optimal throughout pregnancy.
Having a TSH between 2.5-4.87 mIU/L increased risk of a first trimester pregnancy loss. This is important to consider because these levels are considered “normal” pre-pregnancy. The risk of miscarriage continues to increase when TSH levels increase beyond 4.87 mIU/L. (13)
Can I take T3 thyroid medications in pregnancy?
Many clients that pursue natural treatment or who are working with a naturopathic physician may be used to taking a glandular product like Armour Thyroid. This is made most typically from a pigs thyroid that is desiccated. It will contain some T3 and T4.
The values and amounts of T3 and T4 can not be controlled in this product as they are in a synthetic version and because of the variability concerns I do not recommend a product like this in pregnancy.

T3 does not cross the placenta and since baby needs mothers thyroid hormone for about half of the pregnancy, there is a risk baby could be hypothyroid if mother is taking a therapy of combined T4/T3.
Managing thyroid health in pregnancy is an area to work closely with your prescribing provider and have monitored routinely. You may need to adjust dosage throughout the pregnancy to support both you and baby.
Thyroid Treatment in Pregnancy – Summary
Thyroid treatment in pregnancy is very important in outcomes for both mom and baby. The normal lab value reference ranges for TSH are more narrow in pregnancy. Treatment of hypothyroidism is critical to lower risk of outcomes like pregnancy loss. This is an area of medical management where I always recommend the levothyroxine/synthroid prescription offered to you from your provider. With stakes being as high as they are, this isn’t a time to try and do things “naturally”. The prescription treatment is there for a reason.
You can see that hypothyroidism is an important thing to manage in pregnancy. What about periods of preconception and infertility?
What role does the thyroid play in preconception and fertility?
PCOS aside, the thyroid alone can complicate chances of getting pregnant or holding a pregnancy. It’s an area that is under appreciated in most OB/GYN offices and even in some fertility treatment centers that I have had patients who were seen at. Let’s dive into the science.
Fertility, PCOS and Thyroid Conditions
One of the hallmark criteria for diagnosis of PCOS is anovulation or oligo-ovulation. Those are big words to say “not ovulating” or “ovulating in frequently”. It doesn’t take an advanced science degree to realize this poses a problem when you want to become pregnant.
We see in PCOS patients that time to conception is significantly longer than women who do not suffer from polycystic ovary syndrome. Research supports that about 40-70% of PCOS patients will be diagnosed with infertility. Ovulation disorders are diagnosed in 75-85% of PCOS Patients. (14) Only about 30% of the PCOS population is estimated to ovulate periodically.
Infertility is defined by one year of regular unprotected sexual intercourse without conception.
In my time working with hundreds of PCOS patients individually, it was common to have a client that never cycled on her own and only experienced a period bleed when on birth control pills. This type of client never ovulates.
I also saw clients who said every 2-3 months they would get a period. That period could be the result of ovulation without subsequent pregnancy or it could be a shedding of uterine lining due to its weight and bulk.

Brief Menstrual Cycle Lesson & Typical PCOS Cycles
A true menstrual cycle requires ovulation in order for a period bleed to happen. Let’s talk a little bit about the cycle mechanics.
Day one of your cycle is always considered the first day of a period bleed where you have to use a tampon, pad, period cup, underwear, etc. Your cycle length will then be from that day one until the next time you bleed.
In between bleeds in a normal and healthy cycle the body experiences hormonal changes that cause the ovary to release a follicle. This will happen 12-14 days before your next period. That 12-14 day timeline is dictated by your body making progesterone. Once the body realizes conception has not occurred, progesterone levels will swiftly decline and then that signals a period bleed.
You can imagine there is a lot of hormone signaling that has to happen in a specific order for all of this to work. So let’s go back to the idea of a client who has a period every 2-3 months, let’s say her cycle averages 75 days. She is likely ovulating late into that cycle around day 61-63. That is if she is ovulating.
Since a typical cycle ranges from 24-35 days, an individual who cycles regularly would have 11-13 times in a year she would ovulate. Someone who cycles every 75 days has 4-5 times she would ovulate. There is only 5 total days around ovulation that intercourse can lead to pregnancy. So that would mean this PCOS patient would have about 24 days she is fertile every year (365 days). Less than half of the days a normally ovulating woman would (55-65 days).
You can see how her chances of conceiving are just less based on less opportunity. That is assuming in those 2-3 month cycles that she is actually ovulating, which is a big assumption and is something that should be tracked and tested for.
PCOS is not the only reason for delay or absence of ovulation. Having hypothyroidism and even subclinical hypothyroidism can impact the cycle and ovulation. So for those who experience both PCOS and thyroid dysfunction, it can be a one, two punch negatively impacting fertility efforts.
Autoimmune thyroid disease is linked in literature with more difficulty conceiving naturally and with assisted reproductive technology like IUI or IVF.
Fertility Requires More than Ovulation
The sex hormones that regulate and dictate female ovulation and menstrual cycle have a strong connection to thyroid function. In fact, women with hypothyroidism are shown to have lower estradiol levels, progesterone levels, and sex hormone binding globulin levels.
It’s amazing to look at how many different areas of the body have receptors for thyroid hormone. Free T3 has been found in the follicular fluid of oocytes. (15) There are thyroid signal pathways all over the uterus, endometrium, and even impact the regulation of specific types of proteins that are critical in the implantation process. (16)
Low levels of thyroid hormone and high levels of TSH can be linked to severe and irregular bleeding, spotting, insufficient endometrial thickness and anovulation. (17) When treating a PCOS fertility client, one of the main goals I have is to help them to ovulate, however with thyroid dysfunction it is not that simple. There are other issues to overcome as well.
How Can I Advocate for Thorough Lab Testing and Thyroid Treatment with My Doctor?
How Can I Advocate for Thorough Lab Testing and Thyroid Treatment with My Doctor?
A thorough thyroid lab panel would include:
- TSH
- Free T4
- Free T3
- Reverse T3
- Anti-TPO antibodies
- Anti-TG antibodies
Autoimmune thyroid disease is the most common type of thyroid disease and it is typically referred to as Hashimoto’s Thyroiditis. Before there are any changes to thyroid function the thyroid antibodies will show as elevated. Then there will first be subtle changes in thyroid function that may not initially flag the attention of your medical provider.
Keep in mind this is a disease progression. It doesn’t happen overnight. First your thyroid dysfunction is impaired by your own tissue mounting an attack on itself. Slowly this would present as subclinical hypothyroidism and progress overtime to become overt hypothyroidism.
One thing to remember is doctors are interested in what they can treat. If you are seeing a doctor and they typically wouldn’t prescribe levothyroxine when a patient has slightly elevated TSH levels, they may not be interested in pulling a thorough lab panel for your thyroid. Why? It won’t change how they treat or prescribe.
You may need to seek the care of an alternative provider, typically Naturopathic doctors or other functional medicine practitioners will look at the thyroid a bit more holistically and be more primed to take early action.
Who should advocate for more thorough thyroid lab testing?
If you are someone that could check off any of the following, I would encourage you to request a thorough thyroid lab panel:
- you are struggling to ovulate
- never have a menstrual bleed
- spot in between periods
- have high levels of insulin resistance
- have experienced a miscarriage
- are pregnant
- are postpartum and/or breastfeeding
- struggle to lose weight despite great effort
How Can I Convince My Doctor to Run These Labs?
If you are trying to conceive or are pregnant you deserve to see thorough lab panels.
In a study of 1,500 pregnant women in Iran thyroid peroxidase antibody levels were followed along with TSH throughout pregnancy. Of note, the women who had elevated antibodies had a miscarriage rate of 36% compared with those without antibody levels elevated who only had a miscarriage rate of 1.8%. (18)
When you consider that a women with PCOS (especially those who suffer from insulin resistance) have a higher chance of developing thyroid disease and combine it with the knowledge we glean from a study like this, it becomes important to look beyond what are considered routine lab requests.
Unless your doctor sees a high TSH level, they will not typically even run a T4 value, let alone thyroid antibody levels. This is concerning because of the prevalence of autoimmune thyroiditis in PCOS patients and the difficulty patients already encounter even achieving pregnancy. Of course, once pregnancy is achieved we are all hoping to support pregnancy for a healthy mom and baby.
What if the tests come back “normal” or close to it?
Most of the conventional medical world will not consider treating thyroid function or even digging into more thorough lab sets until your TSH is above 4.0-5.0 mIU/L. The problem we face is those levels are already too high for pregnancy.
It doesn’t take a rocket scientist to look at that and see an issue. If you were to conceive and thyroid function needs to increase with pregnancy, it makes sense your TSH will likely go up even higher. Asking to try and tighten TSH levels prior to pregnancy seems evidently prudent.
We see in research that as TSH levels increase above 2.5 mIU/L insulin resistance levels go up. High levels of insulin impact testosterone production at the ovary and impair ovulation. TSH levels of 2.5 or higher increase the risk of miscarriage. (19) Considering both the impact on achieving pregnancy and the increased risk once pregnant, it is worthwhile to at least trial thyroid medication and see it’s impact on cycle regularity and subsequent TSH levels.
With these things in mind, it is worth requesting thyroid support if you are in a position of trying to regulate your cycle, ovulate, conceive or are already pregnant and have a TSH higher than 2.5.
If your TSH comes back normal and you have been able to obtain thyroid antibody values that show to be elevated, it is my recommendation to request your physician consider thyroid medication. We see similar findings not only in the previously mentioned study in Iran, but in a follow up study conducted in Italy.
948 women were recruited in southern Italy who were in their first trimester of pregnancy. Thyroid levels and thyroid antibody levels were routinely tested throughout pregnancy. There were 115 women who had high thyroid antibodies. These women were allocated in a group receiving thyroid medication (levothyroxine) along with another group receiving no medication. There was the additional group of over 800 women who didn’t have elevated thyroid antibodies. The rate of miscarriage was 14% in the women with high levels of antibodies who did not receive the treatment. The group with high antibodies that did receive thyroid medication was only 3.5% while the group that had no elevation in antibodies had a miscarriage rate of 2.4%.
Early and proactive treatment for individuals with PCOS and Hypothyroidism (or even Subclinical Hypothyroidism) makes sense and could alleviate unnecessary time to conception and decrease the risk of miscarriage.
If you are someone that suspects thyroid could be part of the health picture for you, consider starting to track your BBT. That stands for basal body temperature. Tracking BBT can give a window into your metabolic function by way of temperatures.
Using an oral or other internal thermometer take your temperature when still in bed upon waking in the morning and track this in a cycle tracking app. If your temps are routinely lower than 97.0 degrees F or 36.1 degrees C you may have an underactive thyroid.
Checking with a skin thermometer like the wearables on the market including the apple watch, ava, and tempdrop will always report a little lower than the internal temps, so those are not reliable to check for low temps indicating an underactive thyroid .

A Case Study of Subclinical Hypothyroidism, PCOS and Fertility
A Case Study of Subclinical Hypothyroidism and Fertility
I had a patient(we will call her Claire) back in 2018 with routinely regular cycles, signs of ovulation, diagnosis of PCOS, symptoms of hair loss and hirsutism, polycystic ovaries on ultrasound, and lab work revealing higher levels of testosterone. This patient had a thorough work up with a fertility clinic and was working with me.
After timing intercourse for 6 cycles well and no pregnancy, the patient and clinic agreed to do a few rounds of monitored letrozole ovulation induction (even though she was already ovulating). The patient did not conceive in these 4 rounds. Growing weary she was reaching for what alternatives we could consider. After testing progesterone levels and finding them to be adequate we dug into her thyroid levels.
She had a TSH of 3.4 mIU/L, normal levels of free T4 and free T3 but slightly elevated Anti-TPO antibodies. With her symptom picture of hair loss and higher testosterone levels the doctors (and myself) chalked that symptom up to her PCOS diagnosis. I mentioned that her TSH was too high for a first trimester pregnancy time frame and maybe it would be worth asking the doctor to treat her thyroid before she considered any other treatment.
To say her Reproductive Endocrinologist was reluctant would be an understatement, but Claire advocated for levothyroxine and ultimately her doctor agreed. 6 weeks later her TSH was rechecked and it was at 2.1 mIU/L. The low dose of levothyroxine had helped. She also mentioned she had a lot more energy than before.
She and her husband decided not to proceed with any other treatments until they had given her body a chance to acclimatize to her new medication. 1.5 months later (3 months after starting to take thyroid medication) she was pregnant spontaneously. She carried to term and had a beautiful baby girl.
When her husband and she were ready to grow her family again they had a much easier time, and Claire wrote me attributing it to monitoring and treating her thyroid dysfunction.
The classical western medical model doesn’t see a TSH of 3.4 mIU/L as being high. For Claire, it was too high. Was it high because of her PCOS? I’m not sure, but the combination of both was complicating things.
Stories like Claire’s make me want to shout from the roof tops that it is worth advocating for thorough lab work and an open mind where the entire person is treated and not just the diagnosis or labs.
References
1 Polycystic ovary syndrome and thyroid disorder: a comprehensive narrative review of the literature
3 Frequency of Subclinical Hypothyroidism in Women With Polycystic Ovary Syndrome
4 Subclinical Hypothyroidism in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis
5 Association between PCOS and autoimmune thyroid disease: a systematic review and meta-analysis
9 Thyroid Status During Pregnancy in Women With Polycystic Ovary Syndrome and the Effect of Metformin
11 National Instistue of DIabetes and Digetive Kidney Diseases: Thyroid Disease & Pregnancy
12 Reporting Thyroid Function Tests in Pregnancy
14 Thyroid disorders in polycystic ovary syndrome
15 Thyroid hormone concentrations in systemic circulation and ovarian follicular fluid of cows
16 Evidence for triiodothyronine receptors in human endometrium and myometrium
18 Role of thyroid peroxidase antibodies in the outcome of pregnancy
DISCLAIMER
The advice provided in this article is for informational purposes only. It is not meant to augment and not replace consultation with a licensed health care provider. Consultation with a physician, dietitian, naturopathic doctor or other primary care provider is recommended for anyone suffering from a health problem.

I’M CAITLIN JOHNSON!
You are ready to trust your body again. You are ready to fix your hormones and fall in love with your body. Let me show you the way through comprehensive courses to manage your hormones and boost your fertility with PCOS.
Are you
struggling to get pregnant and you don’t know what step to take next. Join Find Fertility today and discover the process hundreds have used to get pregnant and have their dream baby.