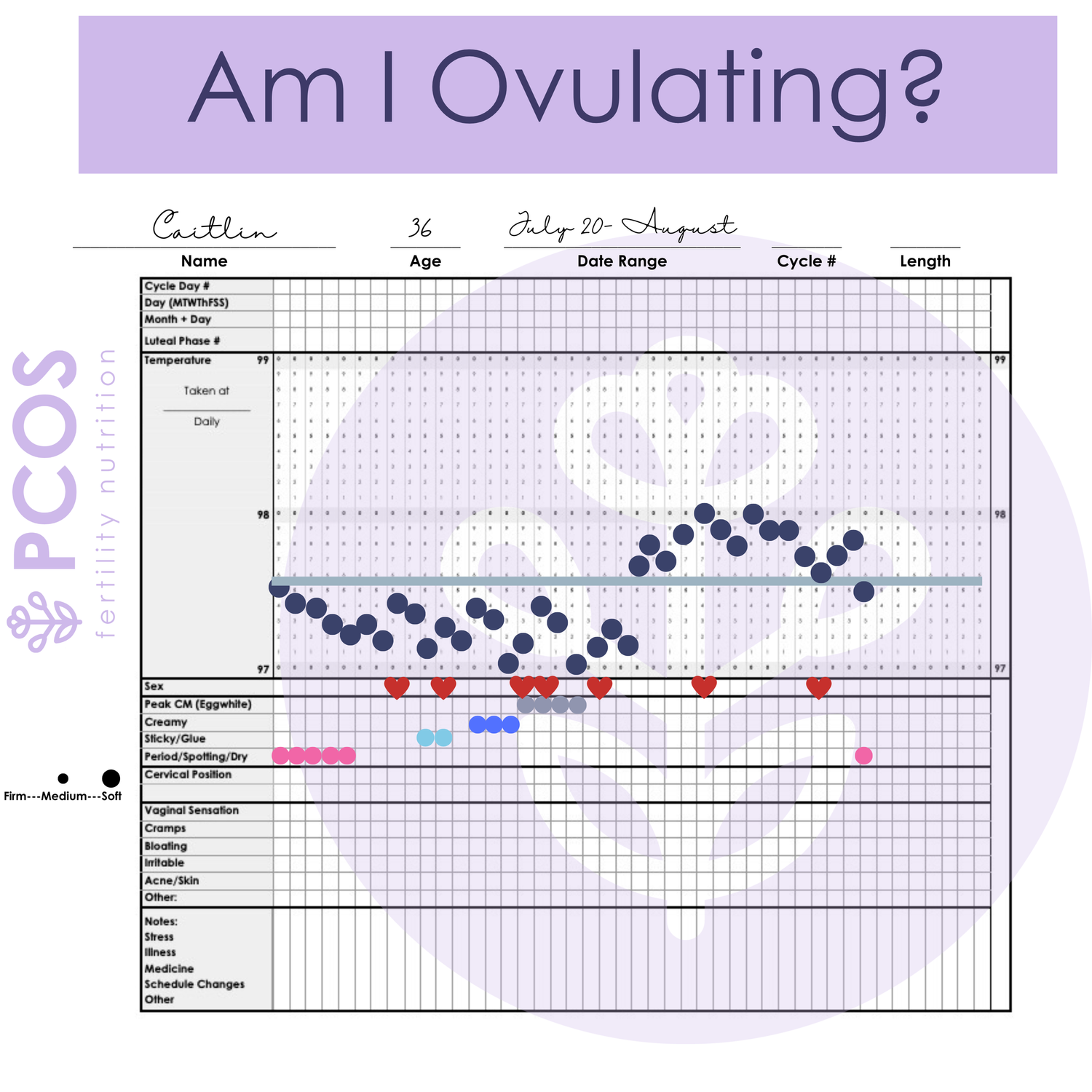
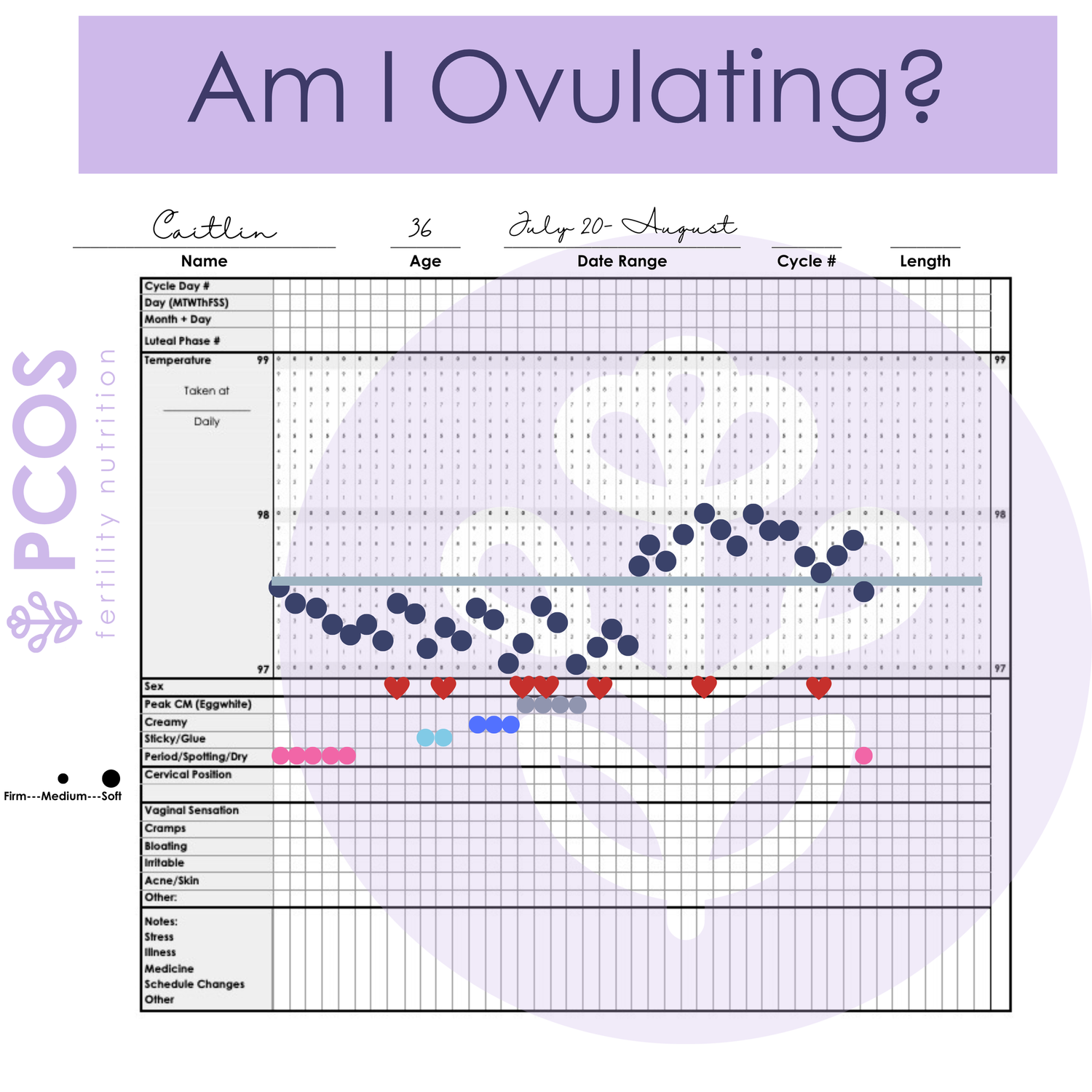
at a glance
Can Keto or Intermittent Fasting Help Me Ovulate with PCOS?
Your doctor told you to lose weight in order to ovulate or get pregnant. No doubt this isn’t the first attempt at weight loss. It’s harder to lose weight with PCOS. Can any popular diets help me get there? What does the evidence say?
There is a lot of debate these days over the most effective way to treat PCOS with diet and lifestyle. It’s generally accepted that diet and lifestyle are the first lines of treatment for PCOS with a focus on obtaining a healthy weight. Yet, a simple search on the internet provides about as many ways to try and lose weight with diet as the number of pounds most of us need to lose(okay, probably more fad diets, but I digress). The diet culture landscape is confusing, leading to many of us with PCOS attempting diets without seeing much success.
While weight loss is an effective tool to help improve ovulation frequency in PCOS – obtaining weight loss can be difficult with the hormonal abnormalities and metabolic dysfunction present in PCOS. It’s often the first piece of advice a doctor will give patients that are trying to conceive, “go lose 5-10% of your body weight.” The other frustrating thing is that weight loss isn’t always appropriate for everyone with PCOS as not all women with PCOS struggle with higher weight.
When weight loss is appropriate, common hormonal abnormalities in PCOS like insulin resistance can make it more difficult to lose weight and promotes higher androgen levels – both of these outcomes make ovulation more difficult.
Is weight loss important for ovulation?
There are multiple hormonal abnormalities common in PCOS that impact how the body matures primordial follicles (baby eggs in your ovary) to the point of ovulation. There is a delicate feedback system between the pituitary gland in the brain and the ovaries. The pulsing of luteinizing hormone (LH) and follicle stimulating hormone (FSH) from the pituitary gland help tell the follicles within the ovary to mature (FSH) and be released from the ovary (LH). This feedback system can be thrown out of balance due to higher levels of luteinizing hormone which needs to come to a higher peak to cause ovulation to occur(1). This chronically high level of LH can also cause women with PCOS to see false positives on at-home ovulation predictor kits (OPKs).
In a small case-control study in Saudi Arabia published in August of 2020 it was reported that there was no difference in LH:FSH ratios between women with PCOS that were obese versus non-obese women. So while many doctors recommend weight loss for women with PCOS patients to stimulate ovulation – this recommendation is over-simplified and doesn’t have evidence in supporting all aspects of hormonal messaging disruptions that are interfering with ovulation.
Losing weight can improve insulin levels which in turn impact other hormones though. So why is this something that gets recommended so often?
Does Insulin Resistance Affect Ovulation?
Insulin resistance is something that affects many of us with PCOS, as many as 7 or 8 out of every 10 women with PCOS. It is a central factor in the symptoms of PCOS including anovulation. Anovulation is just a fancy word for lack of ovulation. Now, you may ovulate with PCOS but still not ovulate regularly, which can also impact fertility. So let’s dig deeper here. How does insulin impact ovulation?
One of insulin’s main jobs is to help get blood sugar into the cell. As the body creates more and more insulin to help move energy(blood sugar) from the bloodstream into the cells of the body – the cells get overwhelmed by the message. It’s like being in a room where the TV is too loud for you, as the sound gets louder and louder you might try to plug your ears – dampening the sound. Cells respond similarly – they stop responding to the loud noise (insulin) and because of that, the message goes unrecognized.

This can happen in most tissues of the body. The ovaries, however, do not become insulin resistant. This is good news in some instances – but in a PCOS body, it is part of the factors that make ovulation more difficult to experience. Too much insulin makes the cells of the ovary (particularly the follicles trying to become the ovulated egg) to instead of making adequate estrogen switch to make testosterone. This can stall follicle development to the point where there is no egg ready for ovulation. Chronically high levels of insulin, cause high levels of testosterone instead of estrogen, thus follicles are not developing correctly and ovulation does not happen. Since this can be traced back to issues with insulin resistance, improving insulin resistance helps improve ovulation.
Popular Strategies to Impact Insulin Levels
We can all agree improving insulin resistance can improve not only weight but hormones that affect ovulation. This is the main focus of many diets: combat insulin resistance. Two very popular strategies of late are keto and intermittent fasting. Both of these eating patterns have been seen to lower insulin levels at least in short trials. Could these be effective ways to help ovulation then?
Let’s consider the Ketogenic Diet:
The ketogenic diet was originally created to help lower the number of seizures in children. It has become popularized in the last number of years for the much broader population as a compelling way to lose weight. There is nothing new under the sun though, this diet was reimagined in a popular trend in the ’90s called the “Dr Atkins Diet”. Now it’s popular under its original name but in a shortened form: Keto.
This diet essentially promotes a very low carbohydrate (typically less than 30 gm per day) intake. In order to eat enough energy the eating patterns contain large amounts of fat and protein. This eating pattern essentially turns your body into a metabolic mode called ketosis. Ketosis is not an efficient way to get the energy to your cells. This inefficiency means you burn more calories to get calories in your food into usable energy in the body. This can have some advantages. However, a diet as high in fat as keto has the unfortunate side effect of being high in calories. Even in a state of ketosis, while eating Keto, you will need a calorie deficit to obtain weight loss. A calorie deficit simply means you need to eat less than you burn.

Many people that promote keto are trying to appeal to the crowds that really want and need to lose weight. It can be pretty appealing to think you can eat an unlimited quantity of bacon and cream cheese. However, it’s really easy to over-eat in a method that is so heavily relying on fat.
In the defense of the ketogenic diet, it does have low carbohydrates it does lead to lower levels of insulin and increased insulin sensitivity. Meaning, that you will have less insulin floating around. Downstream this can affect things like testosterone production and ovulation.
If we are talking about ovulation we are typically considering getting pregnant. It is hard to meet all the needed nutritional requirements for mom and baby on a ketogenic diet. The ketogenic diet is also incredibly restrictive which will lead to diet burnout. It also lacks long-term safety data.
Most studies that we do have on the ketogenic diet in an adult population are very short. In these studies, there are exactly zero performed in PCOS women trying to conceive. While there are things to learn from this eating pattern, it does not get my vote of confidence or meet my recommendation threshold for women with PCOS(which by the way is very high).
Here is the other major downside of the keto diet: you have no wiggle room. Eating one bagel that a co-worker brings to work will pull you right out of ketosis. Ketosis is a state that takes days to get into and one serving of carbs can pull you right out of it. I don’t know about you, but I can’t live my whole life missing carbs.
Intermittent Fasting
So if you have been alive in the last 5 years(which if you are reading this I am assuming you have been) you have heard of intermittent fasting. This is just a fancy way if saying time-restricted eating. This is not new and frankly, if you are alive, you have done this before too. Do you stop eating between dinner and breakfast? That’s an overnight fast and it is also time-restricted eating. The intermittent fasting crowd has taken this to an entirely new level.
What most people mean when they say intermittent fasting:
I only eat within an 8-hour window of the day(typically noon to 8 pm)
I choose to fast for 24 hours twice per week
Now there are different ways to intermittent fast. The first example above could be switched around to eating between 10 am and 6 pm. Essentially this is a 8-hour eating window and a 16-hour fasting window. You can also choose a different eating window like 6 hours or 10 hours.
The second example above is when someone chooses a couple of days per week to not eat at all. This is a less popular option and is not very obtainable for people with real lives, jobs, families, etc.
Like the ketogenic diet, this way of eating is not without its merit. One thing I like about intermittent fasting is that it doesn’t really limit food choices. As long as you eat within your eating window, any food is fair game. This is exactly why I also don’t like intermittent fasting. What you eat does matter: ESPECIALLY IF YOU ARE TRYING TO GET PREGNANT.

There is evidence in the literature that intermittent fasting does improve insulin sensitivity. This makes sense, if you eat within a smaller window of time, your body is making the bulk amount of its insulin in this smaller window of time too. Over a 24-hour period, you can make less insulin. Less insulin = less testosterone = improved ovulation.
The theory is there. The science is there too. However, once again, we don’t have studies in women with PCOS, or even lots of studies with women at all. Less in women of reproductive age and you guessed it, we don’t have a single study on women with PCOS trying to get pregnant.
What Have I seen with Intermittent Fasting and Keto in Practice?
I have seen a number of clients come to me after intermittent fasting and/or keto who have led their bodies into a very stressed-out state and without cycle improvement. This has also really plagued women with a history of eating disorders, including binge eating. Many have felt like these two eating patterns caused a relapse in their eating disorders.
Eat fewer carbs- like a lot fewer- basically, zero (keto) and you’ll switch to burning fat as fuel and you won’t make as much insulin. Eat in very narrow windows of the day or choose entire days where you don’t eat at all a few times a week (intermittent fasting) and your body will make less insulin. While these statements are true they miss really crucial central points. Most studies on keto or intermittent fasting were not done in PCOS, women, or even those trying to manage hormonal conditions or get pregnant. In fact, they are typically done in a male population. Perhaps the most compelling argument is: They aren’t necessary in order to improve insulin resistance or restore ovulation.
How to utilize intermittent fasting benefits without feeling strict or on a diet:
Now, don’t throw the baby out with the bath water yet people. Time-restricted eating has its merits. Instead of thinking so strictly about it, can you stop eating your last meal by 6:30 pm? Can you skip that before-bed snack and have breakfast around 8:30 am the next morning? In a scenario like this, you’ve just created a 14-hour fasting window. That can help improve insulin resistance without feeling super strict or depriving you at all.
Now eating in a pattern like this requires you to also support a healthy circadian rhythm. You can’t stop eating at 6:30 pm and then expect to stay up until midnight without being hungry and going to bed with your stomach growling.
Look at your whole day as it currently is. Can you stretch your overnight fast window slightly? If you currently have a bedtime snack at 9:30 pm and eat breakfast at 7:30 am, can you move your snack to 9 pm and breakfast to 8 am? You just gained an hour there. If over the next month you gain an hour every week, you can gently move your body to a 12-14 hour fast and enjoy the benefits of intermittent fasting without the strict hour requirements.
How to utilize keto dietary strategies without going on a restrictive diet:
Let’s employ some of the tenants of the keto pattern of eating like reducing processed carbohydrates and increasing protein and quality fats. It’s no secret that highly processed grains are sending out blood sugar sky-high. Completely removing carbohydrates from your diet isn’t really the answer either. First what fun would that be and how sustainable is it?
Increasing protein and fat and crowding some of the carbs off your plate? Now that strategy I can get behind. In fact, that’s exactly what I teach in my PCOS+ plate method.
Protein
Colorful Vegetables and Fruit
Oils and Fats
Starches and Carbs as Compliments/Condiments
Does the time you eat your meals affect ovulation?
What a great question! I am so glad you asked. Breakfast absolutely does impact ovulation and let me tell you how. Eating the bulk of your calories at the beginning of the day can help you ovulate. I know you’ve heard that breakfast is the most important meal of the day from your grandma. Seems she really knew what she was talking about.

Eating more of your calories at the beginning of the day can help you ovulate. Now, all I’m talking about here is calories. In a study of “lean” women with PCOS(“lean” meant those with a normal size BMI in the 18.5 to 25 range) they stratified groups into different patterns of eating during the day. It was found that those women who ate the biggest portion of their calories in the morning had the greatest improvement in hormones measured, ovulation restoration and other measurements. 1
Let’s look at what the study looked like:
Participants were divided into two groups who ate 1800 calories per day for 12 weeks. The participants were split into a breakfast group (BK) and a dinner group (D).
The breakfast group ate their biggest meal at breakfast with it being about 980 calories, lunch was 640 calories, and dinner was only about 190 calories. So a really big breakfast and a smaller dinner.
The dinner group had the opposite. The day started with a smaller breakfast of about 190 calories, the same size lunch of about 640 calories, and a large dinner of 980 calories.
Here’s the interesting part – meal size mattered.
The breakfast group saw improvements in insulin resistance and they also saw improvements in testosterone levels and ovulation. The breakfast group had a decrease that was significant in the total area underneath a glucose curve of about 7%, but the total area under the insulin curve decreased by 54%. That is huge! It means that insulin levels were greatly improved by eating the largest meal of the day when they could still work off that energy.
In the breakfast group, we also saw free testosterone decrease by 50%. That’s the testosterone not bound to anything and able to go around the body and affect things, like stopping ovulation from happening or making the hair on the top of your head fall out.
Here is another huge piece ladies: the SHBG (sex hormone-binding globulin) increased by 105%. That means a number could have been low like 30 and increased to 61.5. That is huge. That is the helper that is kind of like Mrs. PacMan floating around and eating up all the free testosterone and other sex hormones, turning them off.
Both groups saw ovulation rates increase in the second month of the trial, but in the third month of the trial, the breakfast group had about 50% of the participants ovulating. And it was statistically significant and much higher than the dinner group.
Why Does Eating a Larger Breakfast and a Smaller Dinner Impact Insulin and Ovulation
When eating the largest meal of the day in the morning you have increased bodily activity to manage increases in blood sugar. You are able to use energy consumed. Your normal activity during the day is higher than in the overnight period so you can use up the blood sugar available from a meal.
Ending the day with the largest meal there are large pulses of energy but bedtime is near and you don’t really need that energy. So that extra energy gets stored as fat. It also has a negative effect on our gut and sleep quality going to bed with a really full stomach(a topic for another day).
It appears both in this study and in others like it that eating larger meals at breakfast and eating less in the later portions of the day insulin levels decrease, fasting glucose levels decrease, and cholesterol and other markers of metabolic syndrome also decrease. In this particular study, we also saw in the BK group that levels of DHEA-S (the adrenal androgen), levels of testosterone, and free testosterone all decreased significantly. We also see that sex hormone binding globulin (our Mrs. Pacman friend that goes around turning off testosterone and other androgen hormones) increased. So we had extra help turning off the androgens that were floating around in the blood increasing symptoms.
These changes both metabolically and hormonally improved ovulation rates. What a simple switch: eating a larger breakfast and less in the evening. This offers a really promising option to try that has very little risk associated with it.
Would This Larger Breakfast Also Help Those Not in the “Lean” PCOS Group?
This was an important question I had when I read the study above because most people with PCOS don’t fit in the lean category(myself included). So I dug into the research and it is true that eating bigger breakfasts and smaller dinners produces similar metabolic benefits in the overweight and obese population, lowering insulin and fasting glucose levels, and HOMA-IR score.
There are many other studies that show (not only in the PCOS population) but in those with weight struggles that eating breakfast can help improve insulin resistance. One particular study with a similar study design tested this theory in those in the obese weight category. This would be someone with a BMI higher than 30.
This study differed to consider the weight loss effects of a similar calorie restriction.2 While both groups ate 1400 calories daily, the calories were either concentrated at dinner time or at breakfast.
In the Breakfast Group (BK)
Breakfast was 700 calories
Lunch was 500 calories
Dinner was 200 calories
In the Dinner Group (D)
Breakfast was 200 calories
Lunch was 500 calories
Dinner was 700 calories
In both groups weight loss was seen – this makes sense with a calorie restriction. Although fasting glucose, insulin, and ghrelin (a hunger hormone) were reduced in both groups, fasting glucose, insulin, and HOMA-IR decreased to a greater extent in the BK group.
Improvement was seen with calorie restriction and weight loss, but there were other differences in the groups. In the breakfast group triglycerides levels went down by 33.6%. In the dinner group triglycerides increased by 14.6%.
Both groups completed an oral glucose tolerance test to test insulin resistance levels after the 12 weeks study. The group that ate a larger portion of calories at breakfast led to a greater decrease in glucose and insulin. This group also lowered ghrelin(the hunger hormone) and hunger scores. They scored higher in feeling satisfied after meals.
When we are talking about improving insulin resistance and improving food “cravings” and hunger – lowering ghrelin is important and improving satiety is important. That’s especially so when we are restricting calories. Breakfast again has many benefits that the dinner-heavy group did not enjoy.
How Can We Apply This Information to Help You Ovulate
In these two studies, you’ll notice we aren’t really talking about all the other things: macronutrient distribution, exercise, fiber intake, specific nutrients, etc. Making sure you are eating enough protein is really critical to help with satiety and insulin levels. Focusing on eating a protein-rich breakfast is always something I consider first when working with people. You don’t need to switch to this overnight, but working towards a bigger, more filling breakfast is a great thing to work towards.
Can you brainstorm 3-5 different protein options you are willing to eat around breakfast time? They don’t even have to be breakfast foods. Here’s a list of things I like:
eggs
cottage cheese
breakfast meats
left-over proteins from dinner
plain greek yogurt
protein shakes
Finding two of those options that you can rotate between and trying to train yourself to eat a bigger breakfast centered around protein would be an awesome goal for this week.

One of the most popular ways people are applying the idea of Intermittent Fasting is to eat between the windows of 12 pm and 8 pm. Thus skipping any intake earlier in the day. If you aren’t convinced yet: eating earlier in the day is important!
It’s important both for your hormonal health and your circadian rhythm health. If that’s a hard message to hear right now, it’s okay. Let’s start slowly moving things that you eat later in the day to earlier in the day. You get the added benefit of not being tempted to have those extra calories be ice cream since that’s not something we typically binge on at 8 am. That and those spicey Doritos are something we are much more likely to reach for at 8 pm. Many of the foods that we “stress eat” tends to happen later in the day and with less nutrition in them. You know what I’m talking about: Cheetos, cereal, popcorn, or desserts. I never seem to hear people say, “I really dove into that salmon and broccoli at 11 pm last night, I was so stressed out.”
In fact, if you were to say to me, I’m just not hungry in the morning, this may actually be why. So not only should you consider taking a few extra bites at breakfast tomorrow, but remember this later in the evening when you aren’t actually hungry but are walking around the kitchen looking for something to eat while you decompress while binging Netflix tomorrow night.
Should I Care About Ovulation Even If I’m not Trying to Conceive?
In short, yes. Ovulation is important for things like metabolic health, bone health, mental health, and even heart health. You do not make progesterone unless you ovulate. Progesterone has a lot of important jobs. Even though your doctor may have put you on birth control, it does not contain progesterone and will not provide the same benefits as those listed above – your body needs to make progesterone in your fertile years or you will pay for it later.

I’M CAITLIN JOHNSON!
You are ready to trust your body again. You are ready to fix your hormones and fall in love with your body. Let me show you the way through comprehensive courses to manage your hormones and boost your fertility with PCOS.
Are you
struggling to get pregnant and you don’t know what step to take next. Join Find Fertility today and discover the process hundreds have used to get pregnant and have their dream baby.